Toenail fungus, also known as onychomycosis, is a common condition that affects the toenails and, in some cases, the fingernails. It results from a group of fungi called dermatophytes, which grow in warm, moist areas. These tiny living organisms feed on the keratin protein inside the nail, leading to discoloration, thickening, and crumbling of infected nails.
Whereas generally it is considered less than common, in reality, toenail fungus cases run into millions worldwide. Though simple in appearance, if left untreated, toenail fungus will more often than not lead to other complications and discomfort; hence, the problem should be addressed with urgency.
This is particularly important because the fungus infection of toenails is painful, shameful, and may result in serious general health problems if it is not treated. It can alter one's life because thickened crumbly nails may make it painful to walk and increase the risks of ingrown nails or secondary bacterial infections. For instance, complications arising from toenail fungus can be rather serious to immunocompromised individuals or those suffering from illnesses such as diabetes.
How Toenail Fungus Develops
The fungi that cause toenail fungus are organisms that love warm, moist environments. Most of the fungi are dermatophytes that belong to a class of fungi that feed on keratin, a protein in nails, skin, and hair. After the fungi enter small cuts, cracks, or separations between the nail and its bed, it starts to multiply and spread underneath the nail.
The fungi that infect the toenails somehow manage to propagate well in humid, warm settings with minimal ventilation. The organisms thrive under conditions when the toes are moist like in sweaty shoes or wet socks. More noticeably, the fungus finds its way from one person to another relatively easily via public places such as swimming pools, lockers, and shared showers.
These fungi feed on keratin in the nail and thereby create a thickening, discoloration, and crumbly edges or grooved patterns during the course of their colonization under the toenail. It may be insidious because a white or yellowish streak appears in the nail that later on progresses to a marked discoloration and distortion. If an untreated fungal infection could therefore result in the spreading to the other toenails, probably painfulness and discomfort will take place with further toenail damage.
Common Causes of Toenail Fungus
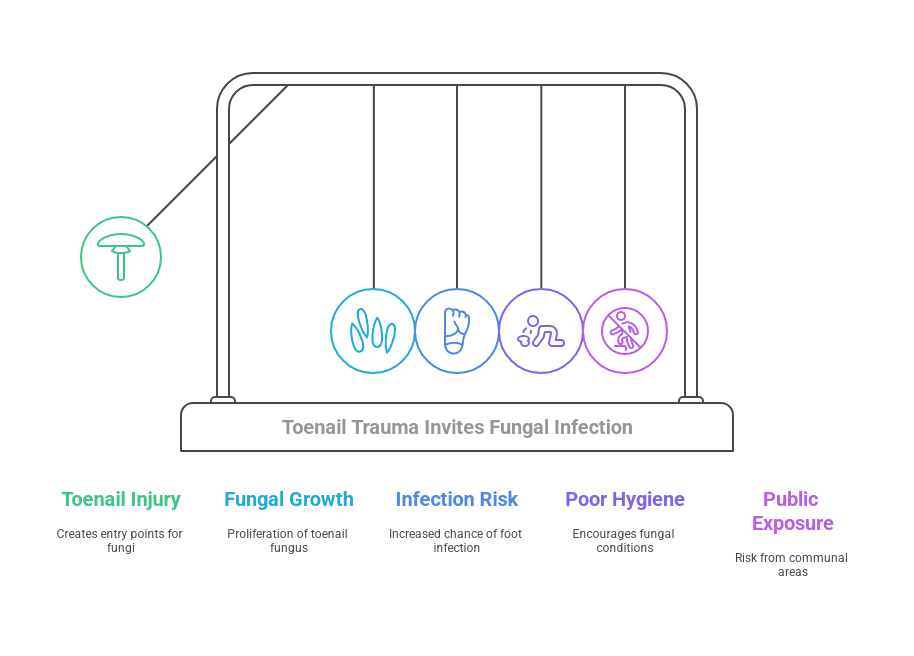
Onychomycosis-or toenail fungus-results from the promotion of the right conditions needed for fungal proliferation. It commonly arises after the toenail has been subjected to a host of injuries or cracking that allows fungi to infiltrate the nail. Trauma from even the seemingly minute condition of stubbing a toe or more severe cases such as onychogryphosis may provide fungi with the means of gaining access to the interior of the nail.
The second major cause is poor hygiene of the feet. Fungi being warm and moist-place-friendly, poor drying after bathing and perspiration will surely invite the growth of these. Further, not changing socks frequently enough or wearing the same shoes for a pretty long time is an invitation to the fungi.
Another major risk factor is walking barefoot in places used by large numbers of people, such as pools, locker rooms, and gym showers. Numerous forms of fungi love these warm, moist environments and coming into direct contact with infected surfaces means coming into direct contact with fungal spores which, given the slightest nick or fissure in the foot skin. It can lead to infection.
Risk Factors of Toenail Fungus
Certain factors can increase your susceptibility to developing toenail fungus. Understanding these risk factors is crucial for taking preventive measures and seeking prompt treatment if necessary.
Medical Conditions: Most of the medical conditions make people susceptible to getting toenail fungus. Diabetes, for instance, reduces circulation and generally weakens the immune system, thereby reducing the chances the body can fight off all types of fungal infections. Other diseases that weaken the immune system, such as cancer treatments and HIV/AIDS, also make a person susceptive.
Age-Related Nail Changes: Changes in nails that come with the normal aging process include thickening, brittleness, and slowed growth. All this provides a field for fungi to develop, thus making older adults more susceptible to toenail fungus.
Tight or Non-Breathable Footwear: Improperly fitted or non-breathing footwear traps moisture and therefore creates a warm, moist environment which is ideal for fungi to flourish. More importantly, the fact that these shoes are worn each day without any opportunity to properly air between uses, will make that environment even more ideal for fungi to grow.
Family History: Fungal infection of the toenails can run in the family, especially if there is an inheritable trait concerning this condition or one lived with someone who has it.
It is also important to establish that one or more of these risk factors does not necessarily lead to toenail fungus; however, knowledge of the same will ensure that a person takes the necessary precautions to minimize their risks and seeks treatment in good time where need be.
Preventing Toenail Fungus
Maintaining proper foot hygiene and taking preventive measures can significantly reduce your risk of developing toenail fungus. Here are some practical tips to keep your feet healthy and fungus-free:
Foot Hygiene
Clean and dry your feet, especially between your toes as fungi like moist, warm parts of the human body.
Wash your feet daily using soap and water; dry thoroughly, particularly between the toes.
Change socks often, using socks made from natural fibers with wicking properties like cotton or wool.
Nail Care
- Trim toenails straight across to prevent ingrown nails, through which fungi can enter.
- A very important tip is never fiddling with your toenails, such as picking and tearing, because it may bring small cracks, allowing fungi to get inside.
- Always disinfect using appropriate cuticle pushers and nail files because fungi can be transferred from nail to nail.
Footwear
- Comfortable and breathable shoes should be used because the material allows dryness and coolness of the feet.
- Alternate between different pairs of shoes to allow each pair enough time to dry out completely before wearing again.
- Wear sandals or flip-flops when out in public to prevent coming into direct contact with contaminated pools, locker rooms and shower floors.
Hygiene in Public Places
- Avoid barefoot walking in shared areas such as the gym, pool, or locker room, given that such moist environments breed fungi easily.
- Bring your own towels. Do not share personal items such as nail files or clippers.
Clean, then disinfect surfaces and equipment before and after use in public areas.
Lifestyle Habits
Getting enough rest, eating a well-rounded diet, exercising regularly, and managing one's stress help to keep the body's defenses up.
- If you have a medical condition like diabetes, follow your healthcare provider's recommendations for proper foot care.
- Quite smoking as it hampers blood circulation, hence making you an easy target of fungal infection.
Some of the preventive measures being integrated into daily life will definitely reduce the development of toenail fungus and keep your toes fit and fungus-free.
When to seek medical advice
Although almost all of them are not serious, there are certain signs and symptoms of toenail fungus that one should show to, or seek advice from, a health professional:
Severe Pain or Discomfort: If there is severe pain or discomfort within the involved toenail or surrounding area, this might become an indication of a more severe infection or complication. Seek immediate consultation.
Thicken, crumbly nails: In the advanced stages of the fungal infection, the toenail may thicken, crumble, or even get brittle. It may be hard to cut and gives more susceptibility to injury or infection.
Nail Separation: The toenail may have started to curve away from or loosen from the nail bed in which it lies. When this happens, it may be indicative of a serious fungus infection that requires further investigation by a doctor.
Infection of Nail Fungus: For nails that have already been infected, one can seek medical help when the fungus has already spread to other toenails or fingernails or when there is reddened, swollen, or oozing skin around the infected nail.
If diabetes is involved, or there is weakened immunity, then the consequences of toenail fungus will be suffered seriously. You fall under this category, then you are advised to visit a doctor or physician for the right concern and treatment.
Persistent or Recurring Infection: If the toenail fungus persists despite self-care measures or recurs frequently, it's time to consult professional medical opinion for better treatment options.
Bear in mind that even though in one's opinion, toenail fungus may be a small thing, giving less attention to symptoms which may be chronic and serious contributes to aggravation. Consult a podiatrist or dermatologist for persistent symptoms, suspicion, or uncertainty related to diagnosis and appropriate treatments.
Approaches to Treatment of Toenail Fungus
Onychomycosis, or toenail fungus, is resistant to treatment and at the same time hard to eradicate. Although this may seem like an easy cosmetic issue, when left unaddressed, it leads to further residual deformation of the nail, pain, and possible complications - mostly for those who have been experiencing either diabetes or weakened immunity. Currently, there are different forms of treatment that may help suppress and potentially clear the fungus.
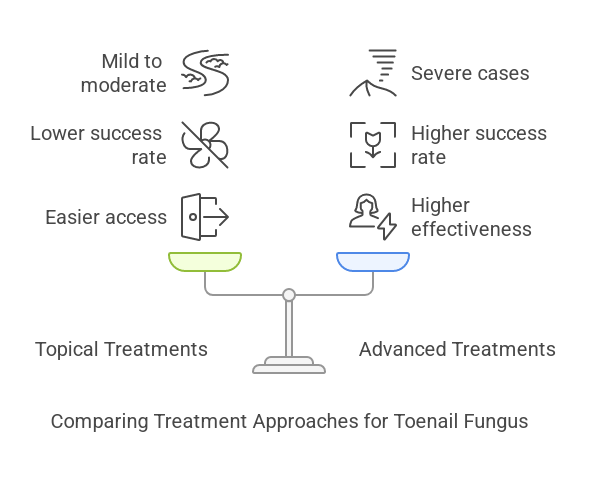
Topical Antifungal Lacquers or Solutions: Lacquers or solutions of various agents such as ciclopirox or amorolfine are applied directly to the nails. They are available over the counter or by prescription. These treatments are usually adequate for mild to moderate disease but have a lower success rate compared to oral therapy, particularly when the infection is far advanced.
Laser Treatment: A new modality that uses focused light from a laser, heating up and killing the fungus in the nail, this solution is painless, drug-free; although it may take several sessions, its success rate in the long run has not been clearly determined as yet.
Surgical or Chemical Nail Removal: The doctor may recommend that the seriously infected part of the nail needs to be removed, or use of a chemical to help in the nail's removal, especially in serious cases or poor circulation of the patients. This allows doctors to apply the anti-fungus treatment directly onto the nail bed.
Combination Therapy: Sometimes, it may require the combination therapy of oral and topical treatment or laser therapy with topical solution for better efficacy besides involving the different aspects of infection.
It is very important to note that this fungus in the toenails is quite resilient and may take several months or even years for proper clearance from the body. Success depends on adherence to the modality of treatment, along with regular follow-ups with the doctor.
Living with Toenail Fungus
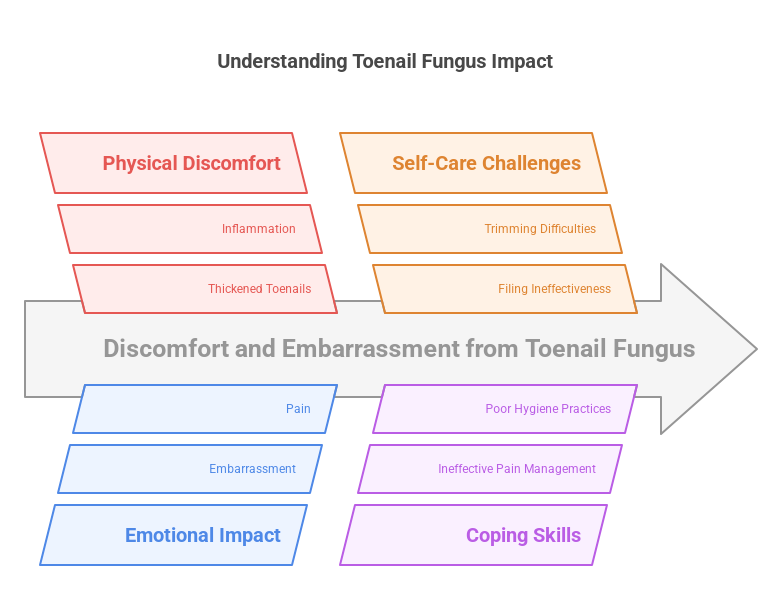
Although toenail fungus is not of a life-threatening nature, it may hugely affect the quality of one's life. These thick, discolored, crumbling nails may cause discomfort, embarrassment, and at times pain. The good news is that the condition is manageable and some of the discomforts associated with the condition can be mitigated with good self-care and effective coping skills.
A key downside in living with toenail fungus is physical discomfort. Thickened toenails press onto the skin surrounding them and cause painful inflammation. Trimming and filing of the nails can reduce such pressure. Wearing properly fitted shoes with space for the toes reduces further irritation.
Maintaining hygiene in the feet is also very important regarding toenail fungus infection control; wash your feet regularly, especially between the toes, and keep them dry. Antifungal powder or spray application keeps it dry and maintains less odor.
Of equal importance is the emotional care that one has to undergo in the process of the fungus. It is unsightly and hence may make the sufferer self-conscious or embarrassed at least in situations that demand showing feet. Self-acceptance and a supportive network can, therefore, help lighten the emotional load.
Cosmetic treatments for the appearance of toenail fungus include the nail polishes or artificial nails created for fungal nails. These are for camouflaging the unsightly discoloration and give one improved confidence.
Along with all that, one must further attend to good living. Wholesome nutrition will help to stabilize the immune system and speed up the recovery process, while regular physical activity will help to avoid stagnation, improve blood circulation, and promote health in general.
Living with toenail fungus is not easy; however, one can make a difference in his quality of life with his ability for self-care. Management of discomfort, hygiene, and emotional strength will see him through till such time it clears up or receives proper treatment.
Myths and Facts about Toenail Fungus
Generally, there are a number of misconceptions associated with toenail fungus. It is simply by knowing the truth that people can understand it and therefore be able to control the growth of such infection. Some common myths and the facts about the toenail fungus infection include the following:
Myth: Fungus of the toenails cannot amount to anything other than a cosmetic problem.
Fact: While fungi infection of the toenails is not seriously dangerous to human health, it can give rise to certain complications, especially in an immunocompromised, weakened individual and in cases of diabetes. If left untreated, it easily spreads to the other nails or even to the skin for further infection, causing discomfort and secondary bacterial infections as a result.
Myth: Fungus infection of the toenails is very contagious and usually picked up casually.
Fact: While toenail fungus is considered a contagious infection, its mode of transmission requires simply skin-to-skin contact with an infected area or the sharing of personal belongings, like towels and nail clippers. It does not usually spread by casual contact in social interaction.
Myth: Toenail fungus only afflicts the elderly or those who are unclean.
Fact: Fungal infection of the toenails is a condition occurring more frequently with increased age and specific states of health; however, it may be acquired at any age in life by individuals who are otherwise healthy and practicing good hygiene. Nail trauma, poorly fitting shoes, and warm moist environments often predispose one to fungal infections.
Myth: Fungal infection of the toenails is easily treated with over-the-counter medications.
Fact: Although a few over-the-counter antifungal treatments can give symptomatic relief in its mild form, toenail fungus is quite hard to be fully taken away, especially in its advanced stage. A full cure may be required with prescription medication or by visiting a professional, depending on the intensity and cause.
Myth: The infected part of the nail can be simply cut away to remove the fungus.
Fact: Trimming or removing the infected part of the nail would give only temporary relief and do nothing to the fungal infection. The nail would grow back again, and the fungus would infect it once again because the fungus is still there. Proper treatment would be required because it would target the root cause of it.
By separating the myths from the facts, one can comprehend toenail fungus better and can make informed decisions on prevention and treatment strategies, along with consultation with healthcare professionals.
When to Seek Professional
Treatment Although mild toenail fungus may improve with self-care and non-prescription antifungal creams, lacquers, and ointments, there are instances where medical attention is warranted. Medical attention from a podiatrist or dermatologist is necessary in the following:
- Onychomycosis is so severe that more than one surface of the nail is involved, totally or subtially. Symptoms that are ongoing or worsening despite good self-management over many months. You have immunocompromised conditions for various reasons, including diabetes, HIV/AIDS, and cancer treatment; all of these might relate to an increased complication risk.
- The infected nail is very painful, uncomfortable, or becoming a bother to carry out daily activities.
- Signs of a secondary bacterial or skin infection such as pus, redness, swelling, and fever.
Persistence of the fungal infection indicates the presence of an underlying predisposing factor. This is how this health condition is usually treated with the following professional treatments: oral or topical antifungal drugs, laser therapy, and even surgical removal of the seriously infected nail.
Only proper diagnosis by a healthcare professional will help rule out other nail conditions that may require different effective treatment.